Acute Bronchitis
What is acute bronchitis?
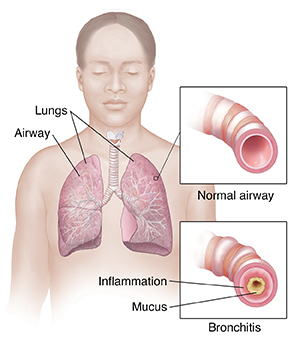
Bronchitis is inflammation of the breathing tubes. These airways are called bronchi. This inflammation causes increased mucus production and other changes. There are several different types of bronchitis. But the most common are acute and chronic. Acute bronchitis is usually due to a viral infection. Another way people describe bronchitis is by calling it a chest cold.
Most symptoms of acute bronchitis last for up to 2 weeks. The cough can last for up to 8 weeks in some people. Chronic bronchitis is a different condition. In chronic bronchitis, the symptoms last much longer. Chronic bronchitis is usually caused by cigarette smoking.
What causes acute bronchitis?
Acute bronchitis is usually caused by a viral infection. This is most often the same viruses that cause colds and the flu. It may also be caused by a bacterial infection, or by physical or chemical agents that are breathed in. These may include dusts, allergens, and strong fumes, including those from chemical cleaning compounds or tobacco smoke.
Acute bronchitis may come after a common cold or other viral infection in the upper respiratory tract. It may also occur in people with chronic sinusitis, allergies, or those with enlarged tonsils and adenoids. It can be serious in people with lung or heart diseases. Pneumonia is a complication that can follow bronchitis.
What are the symptoms of acute bronchitis?
The following are the most common symptoms of acute bronchitis. However, each person may experience symptoms differently. Symptoms may include:
The symptoms of acute bronchitis may look like other conditions or health problems. Talk with a healthcare provider for a diagnosis.
How is acute bronchitis diagnosed?
Healthcare providers can often diagnose acute bronchitis by taking a health history and doing a physical exam. Tests may be done to rule out other diseases, such as pneumonia or asthma. Any of these tests may be used to help confirm a diagnosis:
-
Chest X-rays. This test uses invisible radiation beams to make images of internal tissues, bones, and organs, including the lungs.
-
Arterial blood gas. This blood test is used to analyze the amount of carbon dioxide and oxygen in the blood.
-
Pulse oximetry. An oximeter is a small device that measures the amount of oxygen in the blood. To get this measurement, a small sensor is taped or clipped on a finger or toe. When the machine is on, a small red light can be seen in the sensor. The sensor is painless, and the red light does not get hot.
-
Cultures of nasal discharge and sputum. Tests may be done on the sputum you cough up or on nasal discharge swabbed from your nose. This testing helps find and identify the microorganism causing the infection.
-
Pulmonary function tests. These are tests that help to measure how well the lungs move air in and out. The tests are often done with special machines that you breathe into.
How is acute bronchitis treated?
Acute bronchitis is often mild and does not cause complications. The symptoms often resolve on their own and lung function goes back to normal.
In most cases, antibiotics are not needed to treat acute bronchitis. That’s because most of the infections are caused by viruses. Antibiotics are not effective against viruses. If it has progressed to pneumonia, then antibiotics may be needed.
Treatment is aimed at treating the symptoms and may include:
Don't use antihistamines. They dry up the secretions and can make the cough worse.
What are possible complications of acute bronchitis?
Acute bronchitis can get worse and progress to chronic bronchitis or pneumonia. If this happens, a different treatment may be needed.
Can acute bronchitis be prevented?
Acute bronchitis can’t always be prevented. But there are things you can do to lower your risk for acute bronchitis:
-
Stay away from others who are sick.
-
If you smoke, quit. Ask your healthcare provider for help. They may be able to suggest medicines or other resources.
-
Stay up-to-date on vaccines, as recommended by your healthcare provider:
-
Flu vaccine. Getting a flu shot every year can help prevent both the flu and pneumonia.
-
Pneumococcal vaccine. The pneumococcal shot can protect you from a common form of bacterial pneumonia. Anyone can get pneumococcal disease. But those at the highest risk are children younger than age 2, adults ages 65 and older, people with certain health conditions, and smokers. There are different types of pneumococcal vaccines. Talk with your healthcare provider and your child’s provider about the pneumococcal vaccine. The CDC recommends the vaccine for all children younger than 5 years old, all adults age 65 or older, and certain other people who are at high risk for complications.
When should I call my healthcare provider?
Most often, bronchitis goes away on its own. If your symptoms get worse or don’t get better over time, call your healthcare provider.
Key points about acute bronchitis
-
Bronchitis is inflammation of the breathing tubes. These airways are called bronchi. There are several different types of bronchitis. The 2 most common are acute and chronic.
-
Acute bronchitis is often caused by the same viruses that cause colds and the flu. It may also be caused by a bacterial infection. Or by physical or chemical agents that are breathed into the lungs.
-
The most common symptoms for acute bronchitis include cough, chest soreness, runny nose, feeling tired and achy, headache, chills, slight fever, and sore throat.
-
Healthcare providers can often diagnose acute bronchitis by taking a health history and doing a physical exam. Blood tests, breathing tests, and imaging tests may also be used.
-
In most cases, antibiotics are not needed to treat acute bronchitis. If it progresses to pneumonia, then antibiotics may be needed. Treatment is aimed at managing the symptoms.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your healthcare provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your healthcare provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your healthcare provider if you have questions.